From Fax to FHIR: CMS-0057-F Prior Authorization Rule and API Integration Strategy
- Why the CMS-0057-F Prior Authorization Rule Matters for Digital Health
- CMS-0057-F Technical Requirements: Four FHIR APIs Explained
- FHIR API Integration Opportunities Under CMS-0057-F
- CMS-0057-F Integration Roadmap: From Sandbox to Production
- Key Takeaways
- FAQ: CMS-0057-F Prior Authorization Rule and FHIR API Integration

Why the CMS-0057-F Prior Authorization Rule Matters for Digital Health
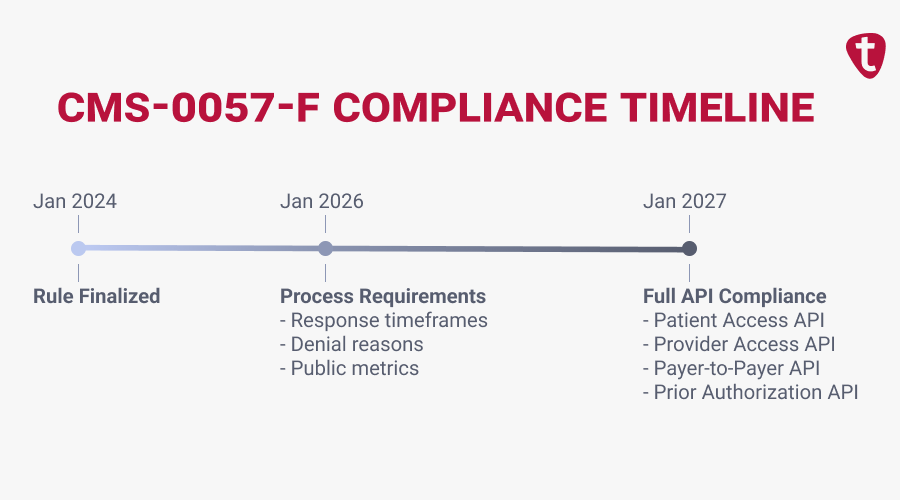
CMS-0057-F is the federal rule that finally forces standardized APIs into prior authorization workflows. Finalized by the Centers for Medicare & Medicaid Services (CMS) in January 2024, it mandates that Medicare Advantage, Medicaid, CHIP, and QHP issuers on the FFEs expose FHIR-based APIs for prior authorization and data exchange. Compliance deadlines start January 1, 2026, with full API compliance required by January 2027.
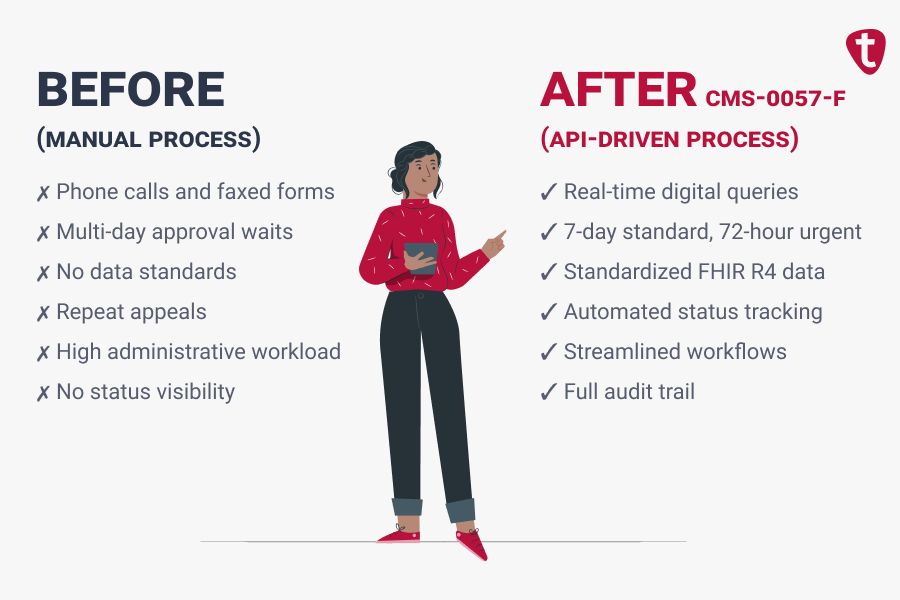
Right now, prior authorization is mostly manual: phone calls between providers and payers, faxed documentation, multi-day approval timelines, and denied requests leading to repeat appeals. For patients, it means delayed care; for providers, administrative burden; and for payers, a cost center they can’t automate because there’s no standardized API to plug into. CMS-0057-F changes that equation.
For digital health companies, this isn’t just compliance news. Covered payers must now build and expose APIs they’ve historically resisted. If your product touches prior authorizations, care coordination, or patient data aggregation, CMS-0057-F makes your integration roadmap more predictable and your addressable market larger.
But predictable doesn’t mean simple. The rule specifies four distinct APIs, each with its own implementation guide. Build to the right spec or risk missing the mark.
CMS-0057-F Technical Requirements: Four FHIR APIs Explained
The CMS-0057-F prior authorization rule mandates four FHIR APIs that payers must implement. Each serves a different part of the data exchange workflow, and each creates different integration considerations for your product.
The Four Required APIs
Patient Access API enables patients to access claims, encounters, and prior authorization status through third-party apps. Payers must include prior auth data within one business day of any status change.
Provider Access API gives providers direct access to patient data held by payers – adjudicated claims, USCDI (United States Core Data for Interoperability) elements, and prior authorization information.
Payer-to-Payer API ensures continuity when patients switch coverage. Payers must exchange five years of patient data, including prior authorization history.
Prior Authorization API is the centerpiece. Providers can determine whether authorization is required, query documentation requirements, and submit requests – all from existing systems.
FHIR Standards and Authorization Protocols
All four APIs build on a common technical foundation:
HL7 FHIR R4 is the data model. You structure prior auth requests, eligibility data, and clinical summaries as FHIR resources (ServiceRequest, Claim, ClaimResponse, etc.). FHIR is extensible – payers can add fields, but the core is standardized.
SMART on FHIR is the authorization layer. It lets users (patients or providers) grant apps permission to access specific data without sharing passwords. Under the hood, it’s OAuth 2.0 with healthcare-specific scopes and workflows.
Da Vinci Implementation Guides define the actual prior auth workflows. CRD (Coverage Requirements Discovery), DTR (Documentation Templates and Rules), and PAS (Prior Authorization Support) specify how to check requirements, gather documentation, and submit requests programmatically.
CMS-0057-F Compliance Timeline
January 1, 2026: Payers must report Patient Access API metrics, implement faster prior authorization response timeframes (7 calendar days standard, 72 hours urgent/expedited), provide specific denial reasons, and publicly report prior authorization metrics.
January 1, 2027: Full compliance for all four APIs.
Common Mistake: Assuming January 2027 means you have plenty of time. Payers are building now, and integration partners are being selected now. Waiting until late 2026 puts you behind payers’ testing and certification cycles.
FHIR API Integration Opportunities Under CMS-0057-F
Once payers expose these APIs, new integration surfaces open for digital health products. The question is which APIs matter for your product and how to prioritize payer connectivity.
- Prior Authorization API enables real-time workflow automation. Your product can check if auth is required, pull documentation requirements, submit requests, and track status – all programmatically. For provider-facing tools, this replaces fax-and-wait with queryable, auditable workflows.
- Provider Access API gives your product access to payer-held patient data: adjudicated claims, clinical information, and prior auth history. If you’re building care coordination, population health, or analytics tools, this API surfaces data that previously required manual requests.
- Patient Access API lets consumer apps pull prior auth status alongside claims and clinical data. If you’re building patient engagement or health record aggregation products, this API now includes authorization information within one business day of status changes.
Decision Framework: Choosing Your API Priority
| If your product… | Prioritize this API | Why |
|---|---|---|
| Automates prior auth workflows | Prior Authorization API | Direct workflow integration, highest friction reduction |
| Aggregates patient records | Patient Access API | Pulls claims, clinical data, and now prior auth status |
| Supports care coordination | Provider Access API | Access to payer-held data for treatment planning |
| Spans multiple use cases | Prior Auth + Provider Access | Covers workflow automation and data retrieval |
Consultant’s Tip: Payers will implement these APIs with slight variations – different endpoints, authentication flows, and custom extensions. Design your integration layer to absorb payer-specific differences through configuration, not code forks. This pays off quickly when you add your fourth or fifth payer.
CMS-0057-F Integration Roadmap: From Sandbox to Production
If you’re building a product that integrates with these payer FHIR APIs, here’s how to sequence your approach.
Phase 1: Technical Foundation (Months 1-3)
Get hands-on with the Da Vinci IGs before payer APIs go live. Stand up a sandbox using public test servers and reference implementations. The learning curve, such as FHIR resource relationships, SMART authorization flows, and IG-specific workflows, takes time. Starting now means you’re ready to connect when payers flip the switch.
Simultaneously, identify which payers matter most for your target customers. Research their developer programs and registration processes – some require months of lead time.
Phase 2: Integration Architecture (Months 3-6)
Design for multiple payers from day one. Your architecture should handle:
- Payer-specific authentication and registration
- Endpoint and extension variations across payers
- Normalized data models that abstract payer differences
- Error handling and retry logic for API reliability
Avoid hard-coding payer-specific logic into your core product. New payer connections should be configuration changes, not engineering projects.
Phase 3: Pilot Integrations (Months 6-12)
Deploy with early customers who have patients covered by your target payers. Real production traffic reveals edge cases that sandbox testing misses – malformed responses, timeout behaviors, data quality issues.
Track integration-specific metrics: API response times, error rates, and successful transaction rates. These inform both your product reliability and your sales narrative.
Phase 4: Expand Payer Coverage (Months 12+)
Each new payer integration should be faster than the last. Your abstraction layer absorbs differences; your team builds pattern recognition. Focus on operational capabilities that scale: monitoring, alerting, and payer-specific support documentation.

When to Bring in EHR Integration Help
Integrating with payer FHIR APIs while also connecting to provider EHRs multiplies complexity. Consider working with a healthcare integration consultant when:
- Your team hasn’t built production FHIR integrations before
- You need to navigate payer developer programs and registration
- You’re balancing payer API work alongside Epic or Cerner connectivity
- Sales timelines are pushing faster than your team can deliver
The best EHR integration consulting companies have built these integrations before and can compress your timeline significantly, especially when you need both payer API connectivity and EHR integration working together.
Key Takeaways
- CMS-0057-F mandates four FHIR APIs by January 2027, replacing fax-based prior authorization with standardized, queryable interfaces.
- Technical stack: HL7 FHIR R4, OAuth 2.0/OpenID Connect, Da Vinci IGs (CRD, DTR, PAS), and SMART on FHIR for EHR-embedded workflows.
- Prioritize based on your product: Prior Authorization API for workflow automation, Provider Access API for payer data retrieval.
- Start now: Build against Da Vinci specs and begin payer developer program registration early – administrative timelines often lag technical readiness.

FAQ: CMS-0057-F Prior Authorization Rule and FHIR API Integration
Standard requests must receive decisions within 7 calendar days. Urgent or expedited requests must receive decisions within 72 hours. These timeframes apply regardless of how the request is submitted – payers can’t claim slower timelines for faxed requests.
CMS requires impacted payers to publicly report prior authorization metrics starting January 2026. These reports provide transparency into payer performance and adoption. Engage with payer developer programs early for visibility into their specific timelines and technical approaches.
Patient Access API is designed for patient-authorized third-party apps – startups building consumer health products can leverage this directly. Provider Access API requires treatment relationships, so startups building provider tools need to work through their provider customers. Your access path depends on whether you’re building patient-facing or provider-facing products.
Most impacted payers are publishing developer portals with sandbox access as they prepare for compliance. Check payer websites for developer programs or contact their interoperability teams directly. Da Vinci maintains public reference implementations you can use while waiting for payer-specific sandboxes.
Enforcement will phase in over time, and some payers may have delays or exemptions. For product planning, focus on the largest payers in your target markets and assume they’ll be compliant by mid-to-late 2027. Build your integration architecture to handle gaps gracefully – fall back to manual workflows when API access isn’t available, rather than blocking features.

