
Table of contents
- Why FHIR Integration Is Make-or-Break for Startups
- Key Use Cases for Startup Interoperability
- Build vs. Buy: When to Hire an Expert
- Healthcare Startup Journey: MVP to Market Integration Roadmap
- Regulatory & Compliance Basics
- Multi-EHR Connectivity Strategy
- AI Readiness Roadmap
- How to Choose a FHIR Integration Partner
- Investor-Friendly KPIs & Proof Points
- Common Healthcare Startup Integration Pitfalls (and How to Avoid Them)
- FAQ: FHIR Integration Help for Startups, Best FHIR Integration Consulting Companies
Why FHIR Integration Is Make-or-Break for Startups
You’ve built a brilliant healthcare product. Clinicians love your demo. Now your first enterprise customer asks: “How do you integrate with Epic?” This is where FHIR integration consulting for healthcare startups becomes truly make-or-break.
FHIR integration consulting impacts three survival metrics:
First, customer acquisition velocity: enterprise health systems won’t sign without proven EHR integration. Your sales cycle ranges from 3 to 9 months as you build connections.
Second, product differentiation: integration depth determines whether you’re a ‘nice-to-have’ tool clinicians use twice or an embedded workflow they can’t live without. Shallow integration means 60-70% churn within 18 months. That’s akin to losing a full day of revenue each week, leaving you to struggle with rebuilding a quarter of your customer base year after year.
Third, investor credibility: Series A investors now expect a clear interoperability strategy. They’ve watched too many digital health companies burn $500K+ fixing integration technical debt.
Consultant’s Tip: Hire focused consultants for 2-3 integrations, reuse patterns, then build internal skills. That way, you shorten learning from 6 months to 8-10 weeks while finding product-market fit.
Key Use Cases for Startup Interoperability
Integration needs vary wildly based on the startup’s function. Here are three specific archetypes and how FHIR solves their friction points.
The Patient-Facing App (Remote Monitoring)
User drop-off during onboarding. Asking a patient to manually enter their medications, history, and demographics results in massive churn.
- Demographic Sync: Use the Patient resource to pre-fill the onboarding flow.
- Medication Reconciliation: Query MedicationStatement to instantly populate their current regimen.
As a result, you transform a 20-minute, error-prone signup process into a 30-second authorization flow (typically using SMART on FHIR). The user trusts the app immediately because it “knows” them.
Clinical Decision Support (CDS) Tool
Common problem is the “Second Screen” fatigue. Clinicians will not use your tool if it doesn’t have the patient’s current vitals or recent lab results.
Your algorithm can run on validated, real-time clinical data rather than self-reported estimates, significantly improving the safety and efficacy of your clinical recommendations.
- Real-time Context: The app launches directly from the EHR (embedded via iframe).
- Data Ingestion: You fetch Observation (labs/vitals) and Condition (diagnoses) resources instantly.
Digital Therapeutic (DTx) with Write-Back
Another common case is when the “Loop” isn’t closed. You treat the patient, but the doctor never sees the results in their workflow.
- Bi-Directional Data: You don’t just read; you write.
- Workflow Integration: You post a DocumentReference (PDF summary) or a CarePlan update back to the EHR.
Then the provider sees your impact without leaving their native environment. This capability is often the trigger for billing reimbursement (CPT codes), as it provides the necessary audit trail for remote monitoring.
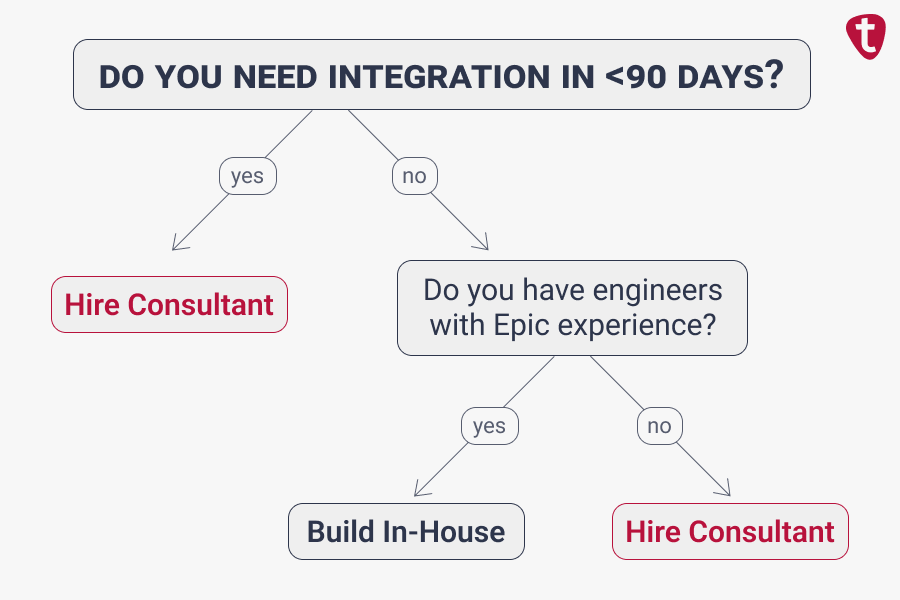
Build vs Buy: When to Hire an Expert
Connecting to EHRs like Epic or Cerner is often the first major bottleneck for health tech startups. The decision to build this infrastructure in-house versus hiring a specialist isn’t just technical – it is a calculation of runway, urgency, and resource allocation. Determine the right path for your stage by analyzing where you are and what resources you’ve got.
Build In-House When:
- You have engineers with prior EHR integration experience on the team
- First customer is 6+ months away, and you can afford the learning curve
- You have 12+ months of runway and can absorb 3-6 months integration timelines
Hire Consultant When:
- First enterprise customer needs Epic/Cerner production connection in <90 days
- You’re navigating health system security reviews and BAA negotiations for the first time
- You need to design a multi-tenant architecture that scales from customer 1 to 10 without rewrites
- Your fundraising timeline demands faster proof points (working integration = credibility)
Consultant’s Tip: If your engineering team estimates the integration will take “two sprints,” they are underestimating the administrative overhead. Hire a consultant to map the architecture and strategy, even if your internal team writes the code
Healthcare Startup Journey: MVP to Market Integration Roadmap
You don’t need “enterprise-grade everything” on day one. You need the right level of Epic/Cerner integration for each stage.
MVP / Design Partner Stage
At this point, “good enough” often means narrow, read-only FHIR access to Patient and one or two clinical resources from a single Epic or Cerner environment. You want to prove you can pull live data for a small set of users while handling PHI safely and logging access.
Pilot with 1-2 Sites
Now you are collaborating with live clinical users. Identity matching, consent flows, and basic audit logs must be solid. You may still be mostly read-only, but adding limited writebacks (for example, visit summaries or flags) becomes realistic.
Scale and Optimization
Finally, you treat Epic and Cerner integration as a repeatable engine. You define standard onboarding steps, expected timelines, and basic SLAs (Service Level Agreements) for uptime and response.
Regulatory & Compliance Basics
Once Epic or Cerner sends PHI into your platform, you’re operating under real regulatory constraints – even if you still feel like a small startup.
In the United States, HIPAA (Health Insurance Portability and Accountability Act) sets expectations around how PHI is handled. Healthcare organizations will expect you to demonstrate:
- Strong encryption in transit and at rest.
- Access controls that enforce least privilege.
- Clear consent and data-sharing logic.
- Audit logs that can answer “who accessed which patient record and when?”
FHIR itself doesn’t make you compliant; it just defines how data is structured and exchanged. The way you design your Epic and Cerner integrations (connection models, authentication, logging, and data retention) is what matters in security reviews.
This is another place where FHIR integration consulting adds value: turning compliance requirements into concrete design decisions and documentation, rather than a last-minute scramble before a go-live.
Consultant’s Tip: Budget 15-20% of your first integration timeline for compliance-related tasks.
Multi-EHR Connectivity Strategy
How to Prioritize Your EHR Integrations
When you are trying to find product-market fit, every week of engineering time counts. You cannot afford to spend months integrating with niche EHRs that your customers aren’t using. The most efficient path to market is a focused assault on the “Big Two”: Epic and Cerner. Here is a timeline for executing a high-impact FHIR integration strategy that follows the revenue rather than the hype.
Epic vs. Cerner Integration Strategy
First FHIR Integration (Month 6-12):
Choose Epic OR Cerner based on your first paying customer. Follow the revenue. Dive deeper and ensure read and write operations are running smoothly. This is your reference architecture.
Second FHIR Integration (Month 12-18):
Add the other major vendor (Cerner if you started Epic, or vice versa). Build an abstraction layer with FHIR integration consulting support. Reuse 60-70% of the first integration work.
Epic + Cerner = 60-70% market coverage. This is sufficient through Series B for most healthcare startups.
Anti-pattern: Trying to support 5+ EHRs before product-market fit. That burns $300K+ and 9 months. Focus on FHIR integration consulting on Epic and Cerner first.
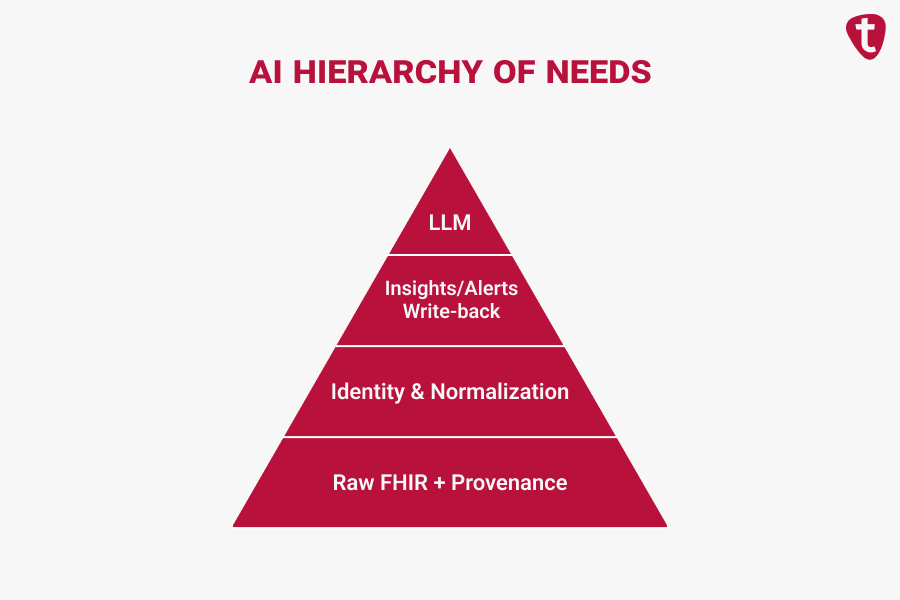
AI Readiness Roadmap
Everyone wants to claim they are “AI-powered.” Investors currently pay 2-3x multiples for healthcare AI companies, creating immense pressure to ship predictive features.
If you want to tell a credible AI story (and investors increasingly expect it), your Epic and Cerner FHIR integration must be designed with data quality and reuse in mind.
A practical AI readiness roadmap looks like this:
- Capture raw and normalized FHIR with provenance.
Keep both the original FHIR resources from Epic or Cerner and a normalized version aligned with your internal data model. Include metadata about source system, site, and timestamps. - Get identity and data quality to “good enough.”
Implement deterministic matching rules for patients and encounters, and add cross-checks to avoid obvious mis-links. You don’t need perfection; you need consistency. - Feed simple insights back into Epic and Cerner.
Before full AI, send basic analytics or rule-based alerts back into the EHR via FHIR – for example, risk thresholds, trend alerts, or follow-up recommendations. This proves that your integration supports closed-loop workflows. - Layer in advanced AI and LLM features.
Once the pipeline is robust, you can add models and copilots that summarize notes, triage cases, or suggest actions. The heavy lifting – trustworthy data in and out of Epic and Cerner – is already done.
Check out our FHIR integration guide to see how to balance raw vs. normalized data for future models.
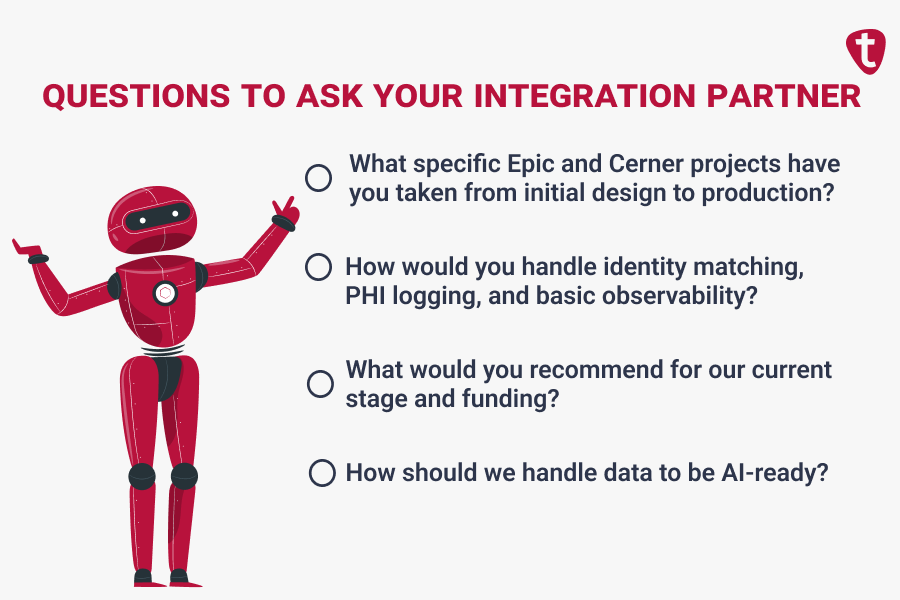
How to Choose a FHIR Integration Partner
There are many consulting companies that “do healthcare.” Far fewer are truly strong at FHIR integration consulting for startups targeting Epic and Cerner, and that’s why you should be looking for a very specific mix of skills.
When you evaluate a FHIR integration partner, ask questions like:
- What specific Epic and Cerner projects have you taken from initial design to production?
- How would you handle identity matching, PHI logging, and basic observability for our use case?
- What would you recommend for our current stage and funding?
- How should we handle data to be AI-ready?
Watch for red flags such as “we’ll just build custom interfaces for every client” or no startup references. Strong partners are honest about trade-offs and will help you pick integrations that are appropriately scoped for Seed, Series A, or Series B rather than over-engineering everything.
Itirra fits this specialized profile: we focus on digital health products, FHIR integration consulting for startups, Epic and Cerner connectivity, and staged integration roadmaps. Ready to stop guessing and start integrating? Contact us to map out a 90-day integration plan that investors will trust.
Investor-Friendly KPIs & Proof Points
Investors generally do not care about the technical nuances of specific FHIR resources. They do, however, scrutinize whether your Epic and Cerner integrations are real, repeatable, and defensible.
The cleanest way to prove that is with a small set of visible, consistent KPIs that demonstrate operational maturity, de-risk the technology, and strengthen your ROI story. Focus primarily on metrics that show production use, speed, quality, and stickiness.
Integration Velocity & Scale
- Time to Live: The average calendar time from signed SOW to first patient live.
- Target: <3 months initially; aim for <4 weeks by Customer #5.
- Live Sites: The number of sites in actual production usage (not just “in implementation” or “pilots in name only”).
Operational Reliability
- Data Accuracy & Completeness: The percentage of error-free exchanges and required FHIR fields populated.
- Target: >98% accuracy; >85% field completion.
- Uptime: Reliability stats for your integration services to prove enterprise readiness.
Business Impact & Stickiness
- Workflow Dependency: The percentage of core workflows in your product that rely on integrated data. This proves integration isn’t just a “sidecar” feature.
- Retention: Churn rates for integrated vs. non-integrated customers.
- Target: <5% churn for integrated customers.
- Cost Savings: Reduction in manual data entry for the client.
- Target: 40-60% reduction.
Common Healthcare Startup Integration Pitfalls (and How to Avoid Them)
A few patterns repeat across Epic and Cerner startups. A few good decisions now can save you significant time and budget later.
Pitfall 1: Supporting every EHR at once.
The usual outcome is scattered effort, slow delivery, and unreliable integrations. A better approach is to pick one primary system (often Epic or Cerner), design an integration layer that can generalize, and then add others deliberately.
Pitfall 2: Ignoring identity until it bites you.
If you leave patient matching to “we’ll figure it out later,” you end up with wrong charts and mistrust from clinicians. Even simple deterministic rules and basic audit checks, defined early, are a huge upgrade.
Pitfall 3: Treating security and IT reviews as paperwork.
When you underestimate these, you get surprised by multi-month delays. Instead, treat PHI, HIPAA, and Epic/Cerner security requirements as a first-class workstream with clear owners and timelines.

FAQ: FHIR Integration Help for Startups, Best FHIR Integration Consulting Companies
A simple, read-only pilot is relatively inexpensive, whereas a bi-directional workflow (writing data back to the EHR) requires more complex engineering and rigorous testing.
Generally, hiring a specialized consultant is significantly more capital-efficient than the alternative: burning months of runway while a full-time engineering team learns the nuances of Epic/Cerner from scratch. You pay for the strategy and architecture upfront to avoid expensive “re-work” later.
The technical connection is often the fast part; the administrative hurdles (security reviews, app registration, and testing validation) cause the delays.
An internal team attempting this for the first time often faces a steep learning curve that can stall a roadmap for quarters. Experienced partners typically compress this timeline by 3x-4x because they anticipate the administrative bottlenecks and use pre-validated architectural patterns, moving you from “kickoff” to “live patient data” as fast as the health system’s IT team can move.
Investors don’t expect a trained LLM at Series A; they expect Structured Data Coverage. You demonstrate readiness by proving your integration captures provenance (where data came from), enforces normalization (mapping to standard codes like LOINC/RxNorm), and maintains strict identity matching. This ensures your future AI models aren’t trained on low-quality data.
Aggregators are excellent for broad, read-only coverage (getting data out). However, if your product requires deep workflow integration, like writing notes back into the chart or launching an iframe inside Epic, you will likely need a direct FHIR connection. A hybrid strategy (Aggregator for breadth, Direct for depth) is often the winning play.
Data shows that “shallow” integrations (where clinicians must leave their workflow to use your tool) lead to 60-70% churn within 18 months. Deep, embedded integrations (Single Sign-On + Write-Back) make your product “sticky,” often reducing churn to <5% because you become part of the daily clinical routine.
Reading data (e.g., pulling a medication list) is low-risk. Writing data (e.g., adding a diagnosis or prescription) changes the legal medical record. Hospitals require significantly stricter security reviews, higher-level OAuth scopes, and complex error handling for write-backs. A consultant can help you scope a “Minimum Viable Write-Back” to avoid getting stuck in 9-month security reviews.

