
FHIR Integration for Digital Health Companies: Complete Guide to Strategy, Implementation & Consulting
Table of contents
- Why You Need This Guide
- Market Landscape 2025 – What It Means for Your Roadmap
- What FHIR Enables for Digital Health
- Integration Options at a Glance
- Multi-EHR Strategy (Epic, Cerner): Sequencing & trade-offs
- AI Readiness from Day One
- FHIR Integration Timeline: From Planning to Production
- Risks & Anti-Patterns (and simple ways to avoid them)
- Metrics That Matter
- Digital Health FHIR Integration: Real-World Case Studies
- Building Internal FHIR Capabilities: Long-Term Strategy
- FAQ: FHIR Integration Consulting & FHIR Integration Help
Why You Need This Guide
Why FHIR integration for digital health companies is now critical
FHIR integration for digital health companies is now a make-or-break capability. Digital health companies today face a fundamental choice that will shape their products’ success over the next five years. The decision isn’t whether to integrate with electronic health records – that ship has sailed. Rather, the question is how to build FHIR (Fast Healthcare Interoperability Resources) integration infrastructure that scales across multiple EHR vendors, supports emerging AI use cases, and doesn’t become technical debt six months after launch.
This is a consulting-led guide for product leaders and architects planning Epic/Cerner paths. Itirra delivers FHIR integration consulting and implementation services – from assessment and architecture to vendor validation, go-live, and ongoing support. The decisions you make about FHIR will determine:
- How quickly you can onboard new customers and close enterprise deals
- How much engineering time you’ll spend on maintenance versus innovation
- Whether your platform becomes indispensable or just another vendor asking for custom data feeds

Market Landscape 2025 – What It Means for Your Roadmap
By 2025, digital health is growing fast and is projected to exceed $1 trillion by 2034. A key driver is interoperability – especially FHIR, which allows smooth data exchange across healthcare systems. Companies adopting FHIR early gain a strong competitive edge, while late adopters risk falling behind. To stay ahead, ensure your systems connect with major Electronic Health Records (EHRs), strengthen security, and use FHIR to enable smarter, data-driven care. Regulators, investors, and health systems increasingly treat FHIR integration for digital health companies as basic table stakes rather than a nice-to-have.
Emerging Trends Shaping 2025
- AI Integration Surge: Over 75% of organizations aim to combine FHIR with AI for smarter workflows.
- Regulatory Shifts: New mandates emphasize data sharing, pushing for faster adoption.
- Investment Focus: Billions poured into interoperable tech signal opportunities for innovators.
Strategic Implications
For digital health companies, this translates into both opportunity and complexity. On one hand, you can reasonably expect that any mid-to-large health system you approach will have some level of FHIR API access available, even if it requires navigating through their IT governance process. On the other hand, differences in implementation guides, API maturity, and feature support across vendors mean that one integration approach won’t fit all. A clear, well-planned strategy is still essential to make FHIR work effectively across systems.
Because vendor implementations and governance differ, teams typically engage FHIR integration consulting to shorten approval cycles, avoid rework, and select the right mix of direct, aggregator, and cloud FHIR for Epic and Cerner.
What FHIR Enables for Digital Health
Understanding what FHIR actually unlocks helps clarify where to invest your integration efforts. At its core, FHIR provides a standardized way to read and write healthcare data across systems that previously required custom HL7 v2 interfaces or proprietary API connections for each vendor. When you look at concrete workflows, it becomes clear that FHIR integration for digital health companies is about much more than just moving data between systems.
- Patient Demographic Synchronization
FHIR makes it easy to pull basic information needed from a patient: name, birthdate, contact details, and identifiers directly from the EHR – patients don’t have to re-enter already existing data.Why it matters:
This simple capability removes one of the biggest sources of frustration in clinical workflows – redundant data entry. When clinicians see pre-filled patient details within your app, adoption rates rise dramatically because it saves time and reduces errors. - Clinical Data Retrieval
FHIR allows secure access to problem lists, medication, allergies, lab results, and vital signs, which is necessary for informed decision-making.Real-world examples may include:
- A chronic disease management platform pulls recent HbA1c values and blood pressure trends.
- A prior authorization tool can automatically fill in diagnosis and medication fields.
- A care coordination app displays scheduled appointments and shows recent visits notes.
The challenge: Different EHR vendors expose different levels of clinical detail through their FHIR APIs. This means your system must handle incomplete or inconsistent data without breaking user experience.
- Bidirectional Integration (Write Capabilities)
Beyond reading data, FHIR also enables writing back into the EHR – adding encounter notes, medication adherence data, or care plans.Why it matters:
This turns your app from a stand-alone tool into an integral part of clinical workflows. When care teams can view and act on information directly within their EHR, your solution becomes part of everyday care delivery rather than an external add-on.Here’s something you should expect: write capabilities typically involve more extensive security reviews, deeper technical integration, longer timelines, and thorough validation to ensure patient safety.
- Real-Time Alerts and Event Subscriptions
FHIR integration supports event-driven updates through vendor-specific notification systems. It lets your app receive alerts about new lab results, patient admissions, or medication changes in real time.Instead of waiting for users to log in and check for updates, care teams can respond immediately to critical events, enabling proactive patient management.
The complexity:
Implementing this feature varies by EHR and often represents the most advanced and technically demanding form of FHIR integration.When to bring in a consultant?
If you need bidirectional writebacks, site-by-site provisioning, or event-driven FHIR Subscriptions, a healthcare/EHR integration consultant helps design the consent model, identity (MPI), and validation plan so clinical workflows don’t break.
Integration Options at a Glance
FHIR integration can take several forms. The right approach depends on your product type, technical resources, and long-term goals.
Decision rule:
- Use direct Epic integration for high-volume sites and writebacks
- Use an aggregator for long-tail coverage
- Use cloud FHIR services for storage/analytics and Bulk FHIR.
Each integration path changes how quickly FHIR integration for digital health companies can scale across Epic and Cerner sites.
API-First Integration: Focuses on using FHIR APIs to exchange data quickly and securely. It gives real-time access to patient information across systems, making it ideal for apps and patient portals that need live updates. This approach is flexible and scalable, but needs good API management and technical expertise.
SMART on FHIR Apps: Enables apps to launch directly within EHR systems like Epic or Cerner using secure OAuth 2.0 authentication. This creates a seamless user experience for clinicians and boosts adoption with least interference.
Cloud FHIR Services: Managed platforms from AWS, Google Cloud, or Microsoft Azure provide secure, scalable infrastructure for storing and processing FHIR data. These aren’t aggregators – they don’t connect directly to EHRs but are ideal for analytics and multi-source data management.
Hybrid Approach: Combine elements based on which EHR vendors you’re connecting to and what data you need:
- Use an aggregator for long-tail community hospitals while maintaining direct connections to Epic and Cerner instances that represent 80% of patient volume.
- Pull read-only data through an aggregator, but handle write operations through direct connections where you need more control.
- Start with aggregators for initial market validation, then migrate high-volume connections to direct integration as revenue justifies the investment.
Not sure which path fits? Schedule a 30-minute consult to compare direct vs. aggregator vs. hybrid for your roadmap.
Multi-EHR Strategy (Epic, Cerner): Sequencing & trade-offs
Planning Your Sequencing
When working with multiple EHRs like Epic and Cerner, it’s important to choose the right order. Most companies start with Epic because of its large market share, then move to Cerner for its strong API support. Each step has trade-offs; for example, Epic offers deep integration but higher costs.
Evaluating Trade-offs
Each EHR (Electronic Health Record) platform brings its own strengths and limitations, so the key is finding the right balance between depth, flexibility, and effort. When deciding your sequencing and integration depth, assess each platform across four dimensions:
- Coverage & Parity: Compare available FHIR resources, read/write permissions, and key differences in how each EHR handles elements like clinical notes, orders, or scheduling.
- Provisioning Friction: Consider how complex it is to register apps, obtain client credentials, promote environments, and get site-level approvals.
- Commercial Leverage: Evaluate benefits such as marketplace visibility, reference opportunities, and contractual flexibility with each vendor.
- Supportability: Review documentation quality, sandbox reliability, API versioning policies, and rate limits – all of which directly affect your development speed and maintenance costs.
Balancing these factors ensures your integration strategy supports both short-term delivery goals and long-term scalability.
Recommended Phased Approach
Rolling out integrations gradually minimizes risks and keeps data consistent across systems.
- Phase 1: Start with Epic for a stable foundation.
- Phase 2: Add Cerner to extend clinical functionality.
- Phase 3: Integrate other providers of EHR systems, like athenahealth, for faster, outpatient-focused support.
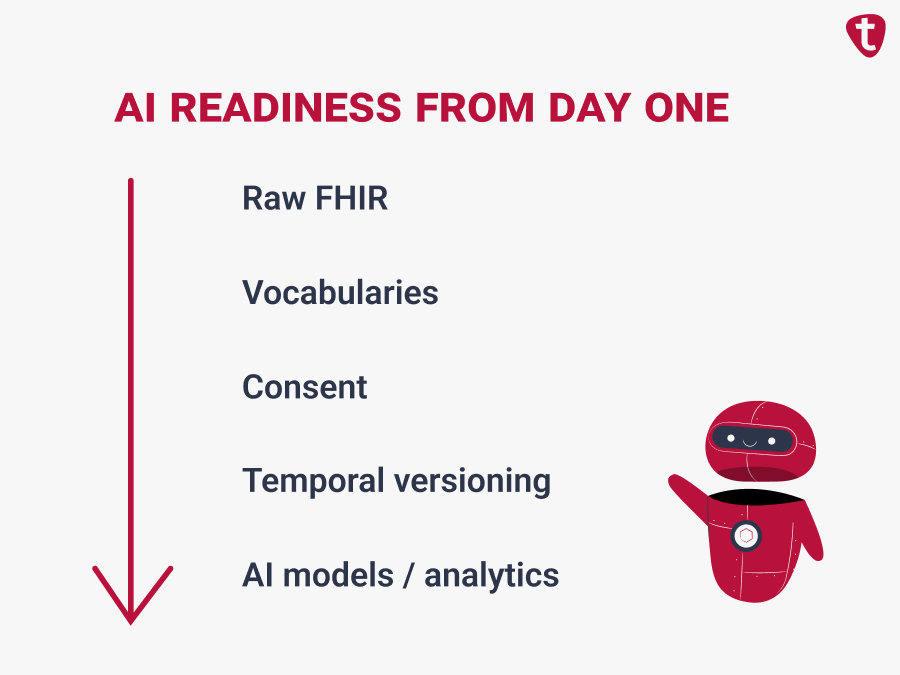
AI Readiness from Day One
If AI is on your roadmap, treat FHIR integration for digital health companies as the foundation of your future data strategy.
FHIR and AI only work well together if you plan for AI from the start. Many teams build FHIR just to “move data around” and later discover the data is too inconsistent, poorly documented, or not consent-aware for real machine learning. If the goal is AI that clinicians and customers can actually use, you need structure, lineage, and guardrails in the pipeline from sprint one.
- Build on a Structured FHIR Data Layer
- Normalize clinical vocabularies (SNOMED CT, LOINC, RxNorm, ICD-10) and store both raw and normalized values.
- Always keep provenance: which health system sent the data, which EHR instance, when it was retrieved, and how complete it is.
- AI models need relationships and history, not just single FHIR resources – medications linked to diagnoses, labs tied to encounters, and longitudinal records.
- Make It Consent-Aware by Design
- Tag every record with consent and purpose of use: who authorized it, what scope was granted, and what it can be used for (care vs. research vs. AI training).
- Enforce this in code and in your data warehouse (not in a spreadsheet later).
- Minimize PHI sprawl – keep PHI only in services that must handle it, and pass references/tokens elsewhere.
- Store Time, Not Just State
Implement temporal versioning so you can rebuild what a chart looked like on a specific date. - Close the Loop in FHIR
If AI creates an insight, it should go back into the workflow.
Write to FHIR resources such as:- Observation for risk scores
- CarePlan for recommendations
- CommunicationRequest for care-team tasks
- Make It Auditable
- Log what was accessed, by whom, and when.
- For LLM-based features, keep prompts and responses for clinical QA.
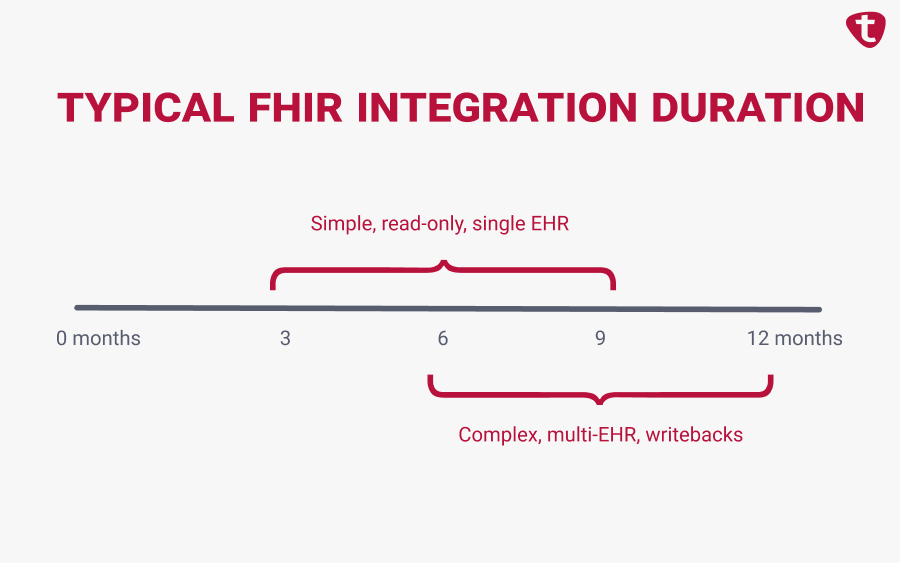
Read-only scope can land in a few months; writebacks, multi-EHR, or stricter reviews push to 3–12 months. Experienced EHR integration consulting typically shortens calendar time by packaging approvals and runbooks.
FHIR Integration Timeline: From Planning to Production
A typical FHIR integration roadmap includes:
- Assessment: Define integration objectives, data scope, and target EHR systems.
- Design: Architect data models, authorization flows, and user experience.
- Development: Build and test FHIR endpoints, SMART app functionality, or API middleware.
- Validation: Perform sandbox testing within EHR vendor environments.
- Go-Live: Deploy production connections and monitor performance.
- Maintenance: Manage version updates, new FHIR resources, and security patches.
A full cycle can take anywhere from three to twelve months, depending on system complexity and vendor responsiveness. However, without a clear roadmap, FHIR integration for digital health companies often turns into a slow, expensive series of one-off projects instead of a reusable platform.
Risks & Anti-Patterns (and simple ways to avoid them)
Even well-planned FHIR projects can fail for the same handful of reasons. Most of them are not about the standard itself but about how teams model identity, deal with EHR differences, and handle scale. Let’s take a practical look at the most common pitfalls below and what to do instead.
| Area / Risk | What typically goes wrong | Better way to do it |
|---|---|---|
| Identity & Data Shape | Patient/provider matching is weak; teams over-normalize and lose the original FHIR resource. | Define an MPI early (deterministic + probabilistic), keep raw FHIR for audit, and build a separate normalized layer with full provenance. |
| EHR & Operational Differences | Teams assume Epic and Cerner expose the same FHIR resources; rate limits and site-level quirks cause failures. | Document per-vendor variations, add contract tests per EHR, and implement retries, idempotency, and rate-limit monitoring from day one. |
| Security, Consent & Compliance | OAuth scopes, consent, and purpose-of-use are added later, leading to certification or privacy issues. | Make pipelines consent-aware (store who authorized what), enforce OAuth in code and warehouse, and audit all access. |
| Architecture & Provisioning | One oversized “integration service,” plus manual onboarding for every new site. | Split into smaller services (auth, data access, mapping, writebacks, monitoring) and script/prototype site provisioning with runbooks in source control. |
Metrics That Matter
To know whether your FHIR integration is actually working, you have to measure both technical health and real-world value. An API that returns 200 but is slow, incomplete, or unused is not a successful integration.
- Reliability & Performance
Check that your APIs are available, fast, and stable. Track uptime, success rate, and P95/P99 response time per resource and per EHR. If latency rises or errors spike, fix that before rolling out to more sites – performance issues scale faster than features do. - Data Quality & Completeness
FHIR is only useful if the data you get matches what your app needs. Measure what percentage of required fields (medications, problems, labs, vitals, encounters) is actually populated, and compare across health systems. If a site’s data falls below your minimum completeness threshold, pause rollout and address it. - Adoption & Workflow Impact
A good integration changes user behavior. Track active users per site, how often integrated data is viewed, and time saved (less copy-paste, fewer context switches). If usage is low, investigate both UX and data relevance – clinicians will not use a feature that shows stale or partial records. - Integration Velocity
Measure how long it takes to bring a new customer or health system live. Over time, this should drop as you reuse mappings, scripts, and runbooks. If every new integration takes the same effort, your platform isn’t getting more leverage. - Business & Clinical Impact
Watch win rate, churn, and expansion for customers with deeper FHIR integration versus those without. Where possible, also track outcome-facing KPIs your buyers care about (faster scheduling, fewer readmissions, better care coordination). A strong integration should help you sell faster and retain better. - Security & Compliance Signals
Because FHIR opens more entry points, tracks audit log coverage, consent mismatches detected/resolved, and access reviews completed. These should be treated like performance metrics – not an afterthought.
Tie all of this to go/no-go rules. If performance slips, data is incomplete, or adoption is low, you pause rollout, fix the root cause, and only then add sites or EHRs. That feels slower today, but it’s cheaper than supporting five broken integrations tomorrow.
Metrics are your guardrails. They tell you whether your FHIR work is creating real value – faster workflows, happier customers, better retention. When you can show a clean line from “better integration” → “more usage” → “better customer outcomes / higher win rate”, it becomes much easier to justify more connectors, more automation, and eventually AI on top. Measure what matters, set thresholds, and your integration layer will stay healthy as you scale.
Digital Health FHIR Integration: Real-World Case Studies
Looking at how teams actually shipped FHIR integrations tells more than theory. These examples show what happens when real customers, real EHRs, and real constraints meet a nice, clean architecture diagram.
Case Study 1: Remote Patient Monitoring – Depth Over Breadth
One RPM (remote patient monitoring) company tried to integrate with every major EHR at once. After months of work on Epic and Cerner, they noticed that most actual deals were with Epic sites. They pivoted and went deep on Epic instead: bidirectional flowsheet writebacks, alerts when vitals worsened, and care-management workflows that felt native. That depth became their pitch, gave them reference customers, and only then did they add Cerner.
Key lesson: Go deep where your customers are, not where the market is theoretically big.
Case Study 2: Chronic Care Platform – Identity Can Break Everything
A chronic care platform started with athenahealth to launch quickly, then added Epic via an aggregator to reach more health systems. Technically, it worked – until production. Patients had different medical record numbers (MRNs) across facilities, so records didn’t line up, and triage staff saw incomplete histories. Adding a lightweight MPI (master patient index) with facility context and probabilistic matching cut mismatches about in half and brought triage times back under five minutes.
Key lesson: In multi-facility environments, building patient matching early or even a good FHIR feed will look “broken” to clinicians.
Case Study 3: Population Analytics – Lineage Wins Trust
A payer–provider venture used Bulk FHIR to build cohorts for value-based care. The tech ran fine, but data stewards pushed back because they couldn’t see how the data was being transformed. The team split the pipeline into protected health information vs. de-identified mirrors and added strict lineage so every feature could be traced to an encounter. Once reviewers could see “this value came from this visit,” approvals sped up.
Key lesson: For analytics, transparency and traceability matter as much as API performance.
What These Cases Show
- Start with speed, grow into complexity. Teams that went live quickly and then added identity, lineage, or direct EHR connections later had fewer bottlenecks than teams that tried to perfect everything up front.
- FHIR is only one layer. The hard work wasn’t calling the API – it was matching patients across sites, putting data where clinicians actually work, and satisfying data/governance requirements. Teams that treated those as core design problems (not afterthoughts) got to real adoption.
- Transparency builds trust. Making data flows visible to stakeholders makes approvals faster and adoption rates higher.
Building Internal FHIR Capabilities: Long-Term Strategy
FHIR should not be treated as a one-off integration task you “finish.” It’s a capability your organization builds and matures over time. Vendors, EHR versions, and regulations will change; if you rely only on external partners, every change becomes expensive. If you grow the skill set inside the company, you control pace, quality, and costs.
Think in terms of a capability, not a project
The goal is to have a team and a platform that can add a new EHR, a new FHIR resource, or a new writeback flow without starting from zero every time. That usually means combining:
- People
- a product manager who understands clinical workflows
- platform engineers who can handle edge cases
- data specialists who own mappings and vocabularies
- security/DevSecOps to keep it compliant
- Environments
- stable test/sandbox setups that mirror real EHR behavior so you can validate before going live
This is how you move from “we can integrate with Epic if we try hard enough” to “we can onboard another Epic site next month.”
Building the internal toolkit
Your team should not re-implement OAuth, retries, and logging for every new project. Give them a small internal SDK or shared services that handle:
- authentication and token refresh
- standardized error handling and retries
- observability (metrics, traces, dashboards)
- contract validation
Add to that a schema or mapping registry so everyone uses the same definitions. Over time, this tooling becomes the backbone of all integrations.
Create living artifacts
Good integration teams keep their knowledge in the system, not in people’s heads. At minimum, you want: a mapping catalog (what we pull, how we normalize it, which codes we accept), a runbook per EHR/site (provisioning steps, quirks, rate limits), and automated test suites (Postman/pytest) to check read/write still works after changes. These artifacts make onboarding new engineers and new customers predictable.
Keep governance lightweight but real
It does not need to be slow or bureaucratic, but it should be clear. Make sure you version and retire APIs instead of breaking existing ones. Review access and consent regularly so you know who can see what. For riskier changes, like new writebacks, AI-generated content, or anything touching PHI, add a quick review step. This keeps your integration secure and stable as it grows.
Invest in people
FHIR evolves, EHRs evolve, and your team should too. Budget for regular training on FHIR updates, USCDI changes, and vendor-specific implementations. Early on, you can lean on consultants, but plan to transition to a dedicated interoperability group as your number of connections grows.
Start with consultants to de-risk first sites and codify mapping registries, contract tests, and promotion checklists. Then transition to an internal interoperability group that reuses the same artifacts to onboard new Epic/Cerner sites predictably.
FAQ: FHIR Integration Consulting & FHIR Integration Help
Yes. 2025+ buyers expect standardized, API-based access, not a collection of custom feeds. FHIR also makes it easier to add new customers without rewriting integrations each time. If you stick to one-off interfaces, your sales and onboarding teams will become the bottleneck.
Bring in a consultant when choosing Epic/Cerner sequencing, designing consent-aware pipelines, planning writebacks, or navigating site approvals. You’ll avoid rework and move through governance faster.
You don’t have to build a full AI platform on day one, but you should store raw + normalized data, keep provenance, and make your pipelines consent-aware. Those are hard to add later once you have millions of records. If you plan for this now, adding risk scores or LLM-powered features later is straightforward.
Simple, read-only, well-scoped work with a cooperative customer can land in a few months. Anything involving writebacks, multiple EHRs, or hospital security reviews will stretch to 3–12 months. The biggest variable isn’t the FHIR spec – it’s how quickly the health system moves.
Optimize for getting a real clinical or operational workflow live – something that pulls or writes data where users actually work. Once that exists, you can justify identity cleanup, AI readiness, and multi-EHR expansion. Shipping something small but real builds trust faster than a big, delayed platform.

